A health benefit exchange should be a competitive marketplace for Americans shopping for health insurance. From 2014 to 2016, only individuals and small groups are eligible to participate in an exchange. Beginning in 2017, larger groups may be permitted to participate.
The health plans offered in an exchange must meet standard requirements for affordability, essential health benefits and consumer protections. The Patient Protection and Affordable Care Act (PPACA) defines four coverage levels:
- Bronze Plan: Covers 60 percent of the actuarial value of covered benefits.
- Silver Plan: Covers 70 percent of the actuarial value of covered benefits.
- Gold Plan: Covers 80 percent of the actuarial value of covered benefits.
- Platinum Plan: Covers 90 percent of the actuarial value of covered benefits.
Exchanges also must include:
In addition, exchanges must provide specific support services, such as:
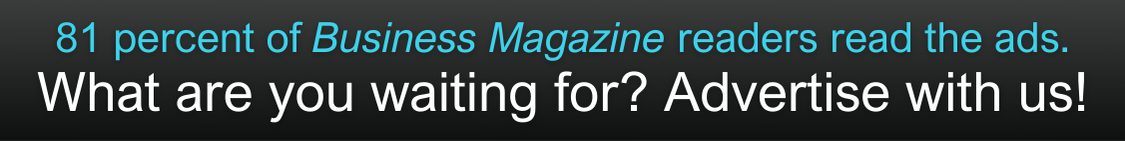
For more information about health benefit exchanges, please contact Patty Smith at 814/833-3200 or 800/815-2660.