Christine Nestor is always on the go.
When she’s not at her busy veterinary practice, she enjoys participating in triathlons, biking, snowboarding and keeping physically fit.
So when an old gymnastics injury was causing back pain a few years ago, Nestor made an appointment with a physical therapist who referred her to Erie neurosurgeon Brad Bellotte, M.D. Bellotte is the chief of Neurosurgery at UPMC Hamot — the largest neurosurgery team in Erie, Pennsylvania.
With UPMC Hamot’s specialization in brain and spine disorders, ranging from arthritis in the neck or lower back, to herniated discs, spine tumors and spinal trauma from accidents, Nestor found a doctor who was knowledgeable in her condition and could provide the treatment she needed. In fact, Nestor first exhausted conservative methods for treatment for a degenerative disc, but after about a year, elected to pursue lumbar fusion surgery using intraoperative computed tomography (CT).
Four weeks after the surgery, Nestor said she decided to go back to work.
“I was careful, but in the first three weeks, you can’t do much more than walk, and I was pretty sore,” Nestor says. “By nine weeks post–op, I had ridden about 80 miles on my bike. It really worked well for me. I’m two years out, and I have no pain.
“Every condition is different,” Nestor adds, “but I had a really great experience.”
At UPMC Hamot, the use of intraoperative CT imaging and other advanced technology is providing a clearer vision for care — and better patient outcomes.
In the case of intraoperative CT, or what Bellotte describes as a “GPS for the OR,” the technology provides greater precision, quality assurance and improved patient safety versus using traditional X-rays.
“Specifically, if we’re working around delicate areas of the spine and putting in instrumentation and metal screws, we can now visualize exactly in 3D where they are going in real-time and verify the results before the procedures are complete,” explains Bellotte. The intraoperative CT also eliminates the exposure to radiation and reduces the chance for a second surgery due to limited views.
So far, UPMC Hamot’s neurosurgeons have performed more than 300 spinal surgeries using the intraoperative CT in the past two years — and positive patient experiences, like that of Nestor. “People hear a lot of horror stories about back surgeries, but they rarely hear the good ones,” says Bellotte. “We’re here to help.”
In addition to spinal surgery, the intraoperative CT is being used for brain surgeries and complicated surgeries to alleviate tremors associated with Parkinson’s disease.
“UPMC Hamot is a real special place with highly trained people,” explains Bellotte. “We’ve got great equipment and people who are willing to advance the field right here in Erie.”
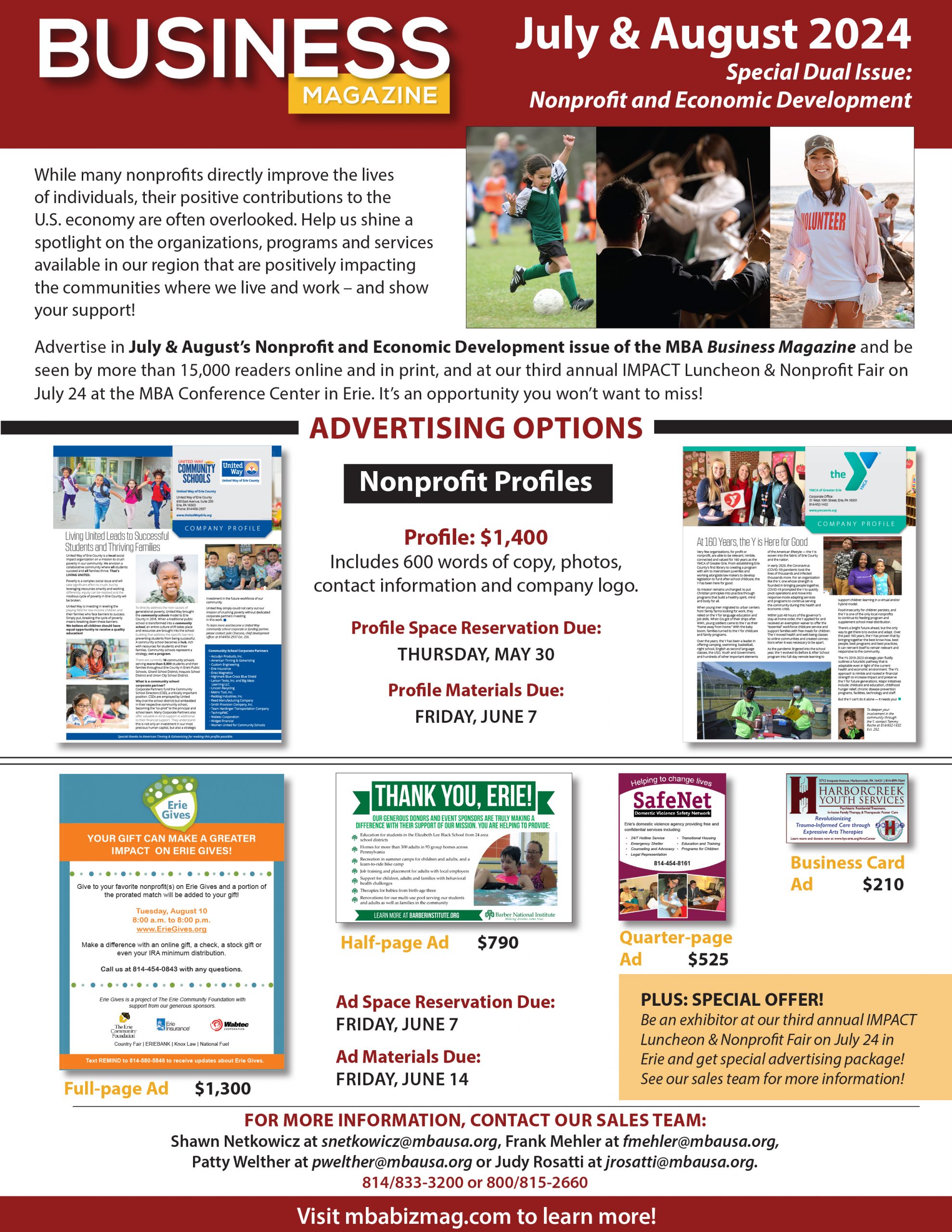
First in the Nation
UPMC Hamot is making great strides in the delivery of care and recently made headlines for its robotic bronchoscopy, as well. In June 2018, UPMC Hamot became the first hospital in the country to use the technology to detect lung cancer earlier.
According to pulmonologist Stephen Kovacs, D.O., co-director of UPMC Hamot’s Comprehensive Lung Center, the ability to diagnose lung cancer earlier is life saving, since patients often show no symptoms until the disease has progressed. Lung cancer is often a “silent killer” as it is more common than the next four cancers combined — colon, breast, pancreas and prostate.
Read more in the February 2019 Business Magazine.