What are some ACA updates that employers should be aware of as we approach 2016?
As we move toward a new calendar year, it’s important to know about the changes that are coming in 2016. Here are the top five:
• Employers with 50 to 99 employees are subject to the employer mandate effective January 1, 2016.
• Individual Medical Out-of-Pocket limit is restricted to the federal cost-sharing limit of $6,850.
• Effective January 1, 2016, employers will not be allowed to reimburse employees through a health reimbursement account (HRA) for premiums of individual insurance purchased in the public marketplace.
• Employers should ensure their wellness incentives are compliant with ACA and ADA requirements.
• Employers should keep in mind that the Cadillac tax is fast approaching (2018), and should modify benefits strategy going forward to minimize the impact.
You’ve mentioned that it will be key for employers going forward to identify ACA opportunities and understand how to maximize them. Tell us more.
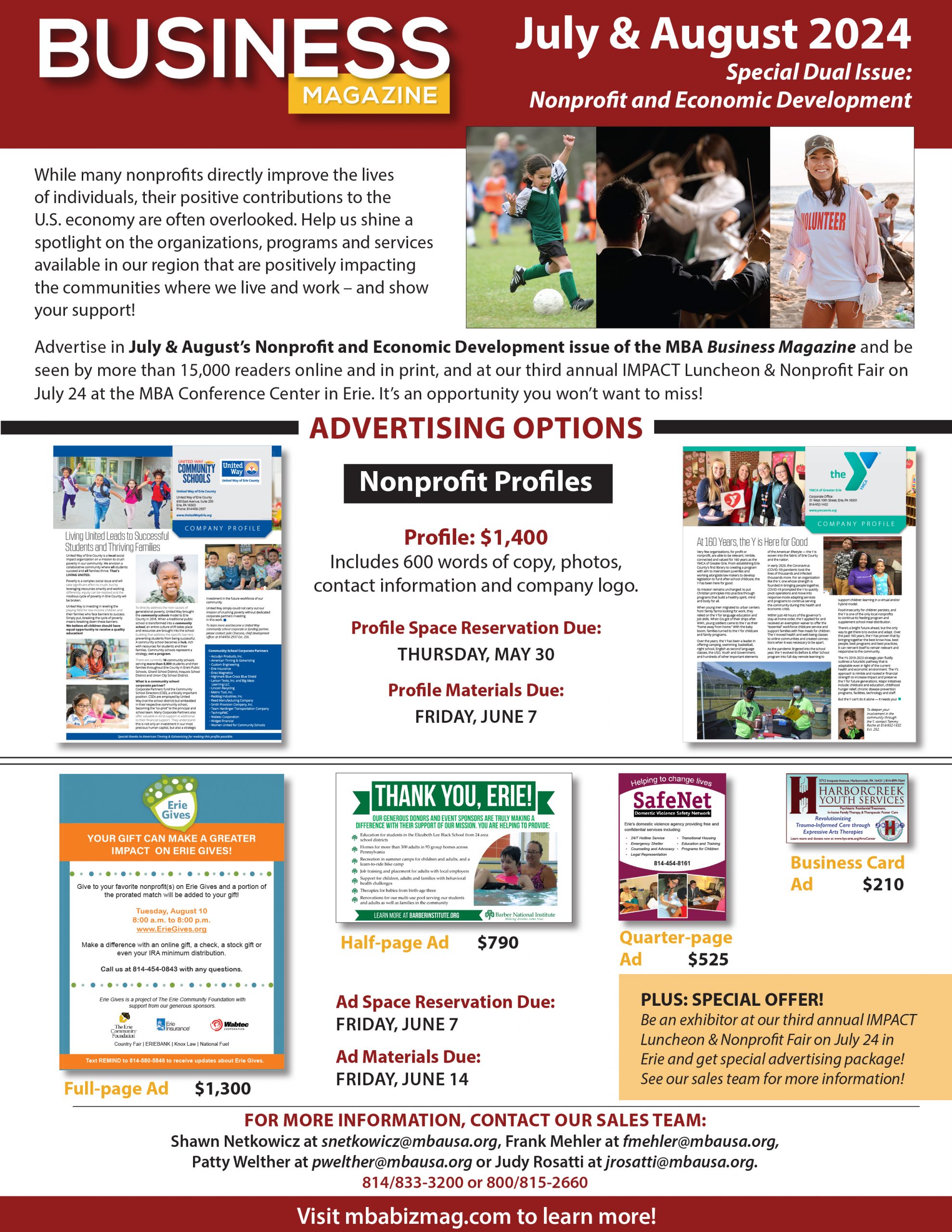
There are more ways to purchase health insurance protection for your employees than ever before. In addition to the traditional group health insurance, there is an ever-growing selection of private exchange solutions (such as the MBA Absolute Choice program), the SHOP small group public exchange option, and the opportunity to direct employees to the public Marketplace for individual insurance plans.
Private exchange solutions, in particular, offer program features that were previously available only to larger groups. Employers should understand their short- and long-term business objectives and how their benefits objectives should align in choosing a direction.
How can organizations use new structures, tools and transparencies to take advantage of emerging strategies, such as private exchanges, defined contribution funding, incentives for healthier behaviors, driving consumerism, targeted messaging and employee advocacy?
By far, the largest driver of health-care costs today is the demand for health-care services. This is a result of unhealthy lifestyles and poor chronic condition management, which account for as much as two-thirds of health-care costs, and lead to greater absenteeism and lower productivity on the job.
Employers, however, can have an impact in the following ways:
• Choose plan designs that get the employee involved from a cost-sharing perspective at the time of service so they see it as spending their own money.
• Promote the use of carrier and private exchange transparency tools that allow the employee to “shop” for health care based on quality and cost.
• Provide financial incentives for employees and spouses to be engaged in their health care, getting biometric screenings to know the current state of their health, and actively participate in programs and coaching to improve the state of their health.
• Communicate with employees regularly about the importance of maintaining healthy lifestyles and effectively treating any medical conditions they have.
• Partner with private exchanges and carriers that include health advocacy resources to help employees navigate through the health-care system.
What’s the best way to help companies and employers prepare for the future under ACA?
Most employers don’t have the resources or the expertise to analyze the complexities of the ACA and accompanying regulations, so it is extremely important to find a partner that will identify potential pitfalls, provide direction for compliance, and prepare you in advance for future ACA provisions. Private exchange solutions offer the most comprehensive and unbiased path toward ACA compliance, combined with the greatest flexibility in designing a solution that meets an organization’s specific objectives and needs.
What compliance issues, such as the approaching Cadillac tax, should businesses be keeping an eye on and why?
The rules around reporting and disclosure under ACA are very complicated and should be reviewed frequently to ensure compliance since the penalties can be severe.
Many, if not all, employers will be impacted by the Cadillac tax eventually since the excise tax threshold is indexed at a much lower rate than current health-care trends. Employers should begin now to build plan design, disease management, and wellness strategies to positively bend the cost curve and minimize the impact of the Cadillac tax.